**Dehydration Signs and Symptoms:**
– Thirst and neurological changes indicate dehydration
– Symptoms worsen with increased total body water loss
– Mild dehydration impairs cognitive performance
– Older individuals may not feel thirsty despite dehydration
– Dehydration is common in the elderly, leading to fatigue
**Causes of Dehydration:**
– Risk factors include hot weather, high altitudes, and chronic illnesses
– Dehydration can result from drug side effects
– Inadequate thirst response in the elderly can cause dehydration
– Excess free water leaves the body through various ways
– Diseases and conditions can disrupt water balance in the body
**Diagnosis and Treatment of Dehydration:**
– Dehydration occurs when water loss exceeds intake
– Dehydration can be life-threatening and lead to seizures
– Differentiate dehydration from hypovolemia for proper treatment
– Proper hydration is crucial for preventing dehydration
– Dehydration can result from normal physiological processes
– Drinking water and reducing fluid loss is effective for minor dehydration
– Solid foods can help replace fluids lost from vomiting and diarrhea
– Correction of dehydration may require oral rehydration therapy
– Isotonic or hypertonic solutions are used for intravenous rehydration
– Avoid injecting pure water intravenously to prevent red blood cell breakdown
**Prevention of Dehydration:**
– Thirst is a good indicator of hydration needs
– Water intake varies based on individual factors
– Additional water may be needed during exercise or in hot environments
– Sweating can lead to significant water and electrolyte loss
– Sodium inclusion in fluid replacement drinks can be beneficial
**Additional Resources and Research on Dehydration:**
– Hydrational fluids
– Terminal dehydration
– Dryness (medical)
– Hypernatremia
– Dehydration Risk factors – Mayo Clinic
– Acute and chronic effects of hydration status on health
– Language guiding therapy: the case of dehydration versus volume depletion
– Hydration and Health Analysis in Nutrition Research
– Hydration and Chronic Kidney Disease Progression: A Critical Review of the Evidence
– Clinical symptoms, signs, and tests for identification of impending and current water-loss dehydration in older people
In physiology, dehydration is a lack of total body water, with an accompanying disruption of metabolic processes. It occurs when free water loss exceeds free water intake, usually due to exercise, disease, or high environmental temperature. Mild dehydration can also be caused by immersion diuresis, which may increase risk of decompression sickness in divers.
| Dehydration | |
|---|---|
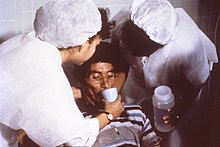 | |
| Nurses encourage a patient to drink an oral rehydration solution to treat the combination of dehydration and hypovolemia secondary to cholera. Cholera leads to GI loss of both excess free water (dehydration) and sodium (hence ECF volume depletion—hypovolemia). | |
| Specialty | Critical care medicine |
| Symptoms | Increased thirst, tiredness, decreased urine, dizziness, headaches, and confusion |
| Complications | Low blood volume shock (hypovolemic shock), coma, seizures, urinary tract infection, kidney disease, heatstroke, hypernatremia, metabolic disease, hypertension. |
| Causes | Loss of body water |
| Risk factors | Physical water scarcity, heatwaves, disease (most commonly from diseases that cause vomiting and/or diarrhea), exercise |
| Treatment | Drinking clean water |
| Medication | Saline |
Most people can tolerate a 3-4% decrease in total body water without difficulty or adverse health effects. A 5-8% decrease can cause fatigue and dizziness. Loss of over 10% of total body water can cause physical and mental deterioration, accompanied by severe thirst. Death occurs at a loss of between 15 and 25% of the body water. Mild dehydration is characterized by thirst and general discomfort and is usually resolved with oral rehydration.
Dehydration can cause hypernatremia (high levels of sodium ions in the blood) and is distinct from hypovolemia (loss of blood volume, particularly blood plasma).
Chronic dehydration can contribute to the formation of kidney stones as well as the development of chronic kidney disease.
